The Role of Neuromuscular Dentistry in Treating Jaw Disorders

The Role of Neuromuscular Dentistry in Treating Jaw Disorders
Jaw pain doesn’t just hurt; it steals your mornings, interrupts meals, and adds a low-grade anxiety to everyday life. When people come to us at Le Denté, they want two things: an explanation that makes sense and a plan that actually helps Neuromuscular dentistry Dubai offers both. It treats the jaw, including muscles, nerves, joints, and teeth, and uses measurable, reversible steps to find a jaw position the body prefers.
Below is a detailed explanation of what’s going on inside the jaw, how neuromuscular clinicians diagnose
TMJ treatment Dubai , the realistic treatment options, what outcomes to expect, and how this approach stacks up against more traditional, sometimes invasive, treatments.
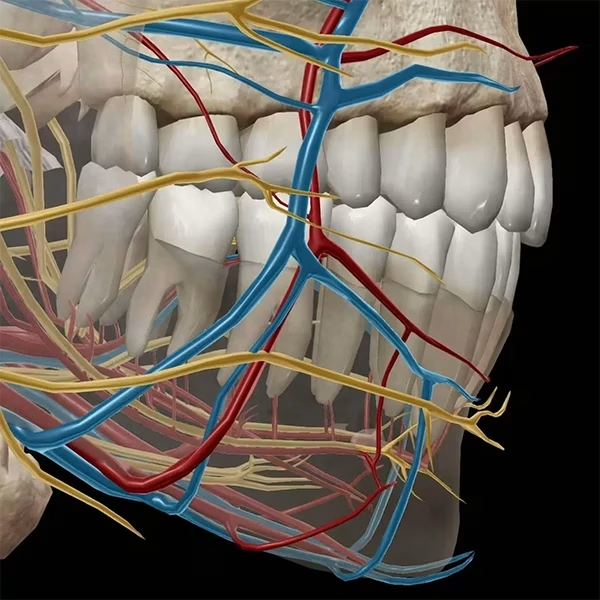
Anatomy & Mechanics: What’s Really Happening When The Jaw Hurts
The temporomandibular joint is deceptively complex. It’s a paired joint that both hinges and slides, cushioned by a small disc, and controlled by powerful chewing muscles (masseter, temporalis, medial and lateral pterygoids). Problems arise when one or more elements in this system fail to work in harmony:
- Muscles become overactive or develop protective patterns from grinding, stress, or an altered bite.
- The articular disc can displace, producing clicks, locking, or reduced opening.
- The joint surfaces can degenerate over time.
- How your teeth meet (occlusion) and how you hold your head and neck change muscle tone and resting jaw position.
- After pain persists, the nervous system can amplify signals so symptoms outlast the original cause.
Understanding whether muscle, disc, joint surfaces, or nervous system changes are the main driver is critical because each requires a different treatment pathway.
What is Neuromuscular Dentistry?
Neuromuscular dentistry looks for a jaw position that minimizes muscle strain and optimizes joint function. Rather than guessing a “proper bite” from tooth marks, this approach uses objective measurements — muscle activity, jaw motion tracking, and low-frequency muscle relaxation techniques to locate where muscles relax and joints move most smoothly. The aim is functional harmony: a bite that the muscles, joints, and nervous system accept and maintain without constant strain.
How Neuromuscular Dentistry Diagnoses TMJ Disorders
Diagnosis combines careful listening with reproducible data:
- Surface EMG (sEMG) measures resting and working muscle electrical activity to spot hyperactivity or imbalance.
- Jaw tracking records movement paths and reveals deviations, deflections, or a limited range.
- TENS (therapeutic low-frequency stimulation) gently relaxes overactive muscles and can help reveal a more comfortable resting jaw position.
- Imaging (MRI for discs, CBCT for bone) is used selectively to confirm structural issues.
- Clinical exam integrates palpation, range of motion, joint sounds, and occlusal assessment.
These tools help separate muscle-driven pain from true structural joint disease — a distinction that changes the treatment approach.
Treatment Modalities in Neuromuscular Dentistry For TMJ
The philosophy is simple: start with the least invasive, reversible options and only proceed to permanent changes when objective stability is demonstrated.
- Education and self-management. Posture coaching, diet modification (soft foods during flares), sleep hygiene, and strategies to reduce clenching are foundational.
- Physical therapies. Targeted exercises, myofascial release, and guided stretching reduce muscle tension and improve mobility. We often coordinate care with physiotherapists.
- Neuromuscular orthotics (appliances). Custom removable appliances set to the neuromuscular position protect teeth, unload muscles, and act as a diagnostic tool: if symptoms improve, we have a reproducible target.
- Muscle-modulation tools. TENS, biofeedback, and, when appropriate, adjuncts like dry needling or low-level laser help change muscle behavior.
- Definitive restorative work (only after stability). If the neuromuscular position proves comfortable over time, restorative steps such as conservative crowns, onlays, or orthodontic alignment are planned to support that position.
- When needed: targeted interventions. If imaging shows structural pathology (severe disc displacement unresponsive to conservative care, infection, ankylosis), surgical or joint procedures may be considered as a last step.
At Le Denté, we treat the orthotic as both therapy and test: it tells us whether a particular jaw position relieves symptoms before we alter teeth permanently.
Symptom Relief and Functional Outcomes
When diagnosis matches treatment, outcomes are tangible: reduced muscle tenderness, fewer tension headaches, smoother opening without locking episodes, and improved chewing comfort.
Some patients notice relief within weeks of wearing an orthotic and doing exercises; others require months of muscle re-training before the position is stable enough for restorative work. Consistency matters: nightly appliance wear, adherence to exercises, and addressing contributing factors (sleep quality, posture, stress) make the difference between temporary relief and lasting change.
Comparing Neuromuscular Dentistry with Traditional TMJ Treatments (Invasive vs. Noninvasive)
Both neuromuscular and traditional TMJ care share noninvasive tools — splints, physiotherapy, anti-inflammatory medication — but they diverge in emphasis and sequencing.
- Diagnostic approach: Neuromuscular care leans on objective muscle and motion data before recommending permanent changes. Traditional approaches sometimes prioritize symptom control or imaging findings without the same physiologic mapping.
- Noninvasive-first philosophy: Neuromuscular protocols intentionally exhaust reversible options and verify improvement before irreversible dental work. Traditional pathways may move to occlusal equilibration or restorative changes earlier in selected practices.
- When invasive treatments appear: Traditional TMJ management includes procedures such as arthrocentesis, arthroscopy, intra-articular injections (steroid or hyaluronic acid), and open joint surgery for structural problems. Neuromuscular clinicians typically reserve these for clearly documented joint pathology after conservative measures fail.
- Practical result: Neuromuscular care reduces the risk of unnecessary irreversible dental work and aligns treatment to what the patient’s muscles and nervous system actually prefer. That said, well-coordinated care can blend both philosophies when structural joint disease objectively demands invasive intervention.
Closing Thoughts
If your jaw problem is interfering with daily life, choose a clinician who measures as well as listens. Neuromuscular dentistry brings objective clarity to a symptom complex that’s often subjective and confusing. It favors reversible, evidence-driven steps and only commits to permanent changes when stability is proven.
If you want a careful, staged path that prioritizes function before definitive restorations, schedule a neuromuscular evaluation with us at Le Denté and see whether appliance therapy and muscle retraining give you the relief you need. Learn more at https://www.ledente.com/.
FAQs
1. Will wearing a neuromuscular orthotic cure my TMJ permanently?
An orthotic is often therapeutic and diagnostic. Many people experience long-term relief with ongoing appliance use plus behavior change. For others, it’s a step toward restorative treatment that supports the comfortable jaw position.
2.Are the tests – EMG and jaw tracking – painful or risky?
No. These tests are noninvasive: surface sensors and small tracking devices record muscle activity and motion. They’re safe, painless, and help target treatment more accurately.
3.How soon can I expect to notice improvement?
Some patients feel muscle relaxation and less pain within a few weeks of starting appliance therapy and exercises. Meaningful, stable functional changes usually take several months of consistent therapy and monitoring.
4.When is surgery the right option?
Surgery is for confirmed structural problems, including advanced joint degeneration, ankylosis, or persistent internal derangement, and only after conservative care has been tried and objective data support surgical benefit.
5.Can neuromuscular dentistry help headaches and neck pain?
Yes. When headaches and neck symptoms are driven by chronic jaw muscle tension or an imbalanced bite, neuromuscular approaches that reduce muscle hyperactivity often reduce those associated symptoms as well.
If you’d like a focused neuromuscular assessment, Le Denté can map your muscle activity and jaw motion, trial an orthotic, and outline a clear, staged treatment plan so you know every step before committing to permanent changes.